We are excited to launch an all-new educational feature – Facets of ME! We will be diving into the multiple facets of ME/CFS including symptoms, comorbidities, practical tips, and more. Our goal is to take the first Friday of each month and delve into one particular facet of ME in a way that is easy to understand. It will be shared on our site and through social media. We hope to lead a great community conversation that will help all of those with ME, including those who are new to ME after COVID19, to better understand the condition.
We can share our hard-won knowledge with one another as well as the wider world to help educate about this illness. People with ME (or people who suspect they might have ME), caregivers, allies, healthcare practitioners, fellow spoonies, and the general public are all welcome to join in by responding to posts and sharing across all social media channels!
We have always worked to build resources for people with ME and continually reach out to those new to ME/CFS. That need is growing exponentially due to the pandemic and the millions more that are coming into our community. New projects like #StopRestPace, #12DaysOfPacing, and now #FacetsOfME are one way we hope to help mentor those new to the disease and keep supporting our long-term community members as well.
Our very first #FacetsOfMe will be this Friday – February 4th! We can’t wait to see what knowledge the community has to share with one another! There is a wealth of knowledge from our lived experiences and we know this will be valuable to many!
Facets of me: post-exertional malaise
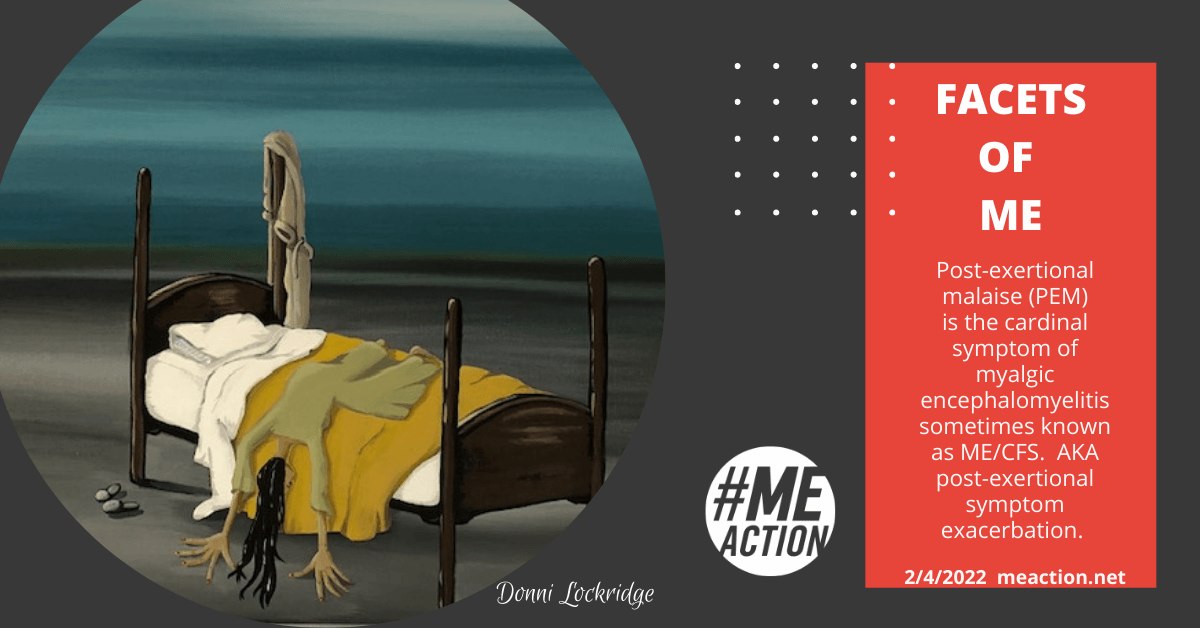
It is time for our very first Facets Of ME! When discussing the facets of ME, it seems almost impossible to start with anything other than the cardinal symptom of myalgic encephalomyelitis — post-exertional malaise (PEM). You might also see it called post-exertional symptom exacerbation or post-exertional neuroimmune exhaustion.
Okay, but what is it really? What does it feel like? How do those who experience it describe it?
PEM “refers to a worsening of ME/CFS symptoms after minimal physical or mental exertion, which can be delayed 24-72 hours or more.” – MEpedia
The more severe episodes of PEM are often called a “crash” by people in our community. A crash in myalgic encephalomyelitis/chronic fatigue syndrome is a “temporary period of immobilizing physical and/or cognitive exhaustion” resulting from post-exertional malaise. – MEpedia
It is not the same as being more tired than normal after activity. It is not the achiness you can get when you are building up muscles and increasing flexibility. It is not something easily cured by a good night’s sleep.
Jaime Seltzer, #MEAction’s Director of Scientific and Medical Outreach, shared in a recent interview with Infection Control Today: “There is now abundant research showing that pushing through this disease not only doesn’t work, but it appears to make patients worse off, possibly in the long term. Post-exertional malaise appears to be a metabolic or immune reaction or both. It is not possible to simply push more and more exertion on the patient and have them regain ability.
Community Descriptions of PEM
It can be hard to explain if you have not experienced the full body assault that is PEM but we are going to try with help of examples from the community. We would love to hear your examples as well.
Sandra
“PEM is just like someone flipping a switch and every last bit of energy you have is completely drained away. When I have a rare good day I am completely surprised at how light my body feels — like I could float away. When PEM strikes, I feel like lead has been pumped into my veins.”
Jessica
“I feel awake but comatose. It hurts to move. I CAN’T move. My body is just done and there is nothing my mind can do about it. It’s like my body is a magnet to the bed. The pull of gravity seems heavier. It feels as if I just ran a marathon, except I didn’t.”
Lucy
“My husband asked me to explain how I feel when PEM hits…all I could think of was to liken it to being weighed down so heavily, that I can’t find the way to move or speak properly. I can see things going on, but processing takes ages, and speech goes. My jaw starting to hurt is often the first symptom of a PEM flare.”
PK
“It’s a strange and varying feeling, which is why we have trouble pinpointing it. But even since my beginning stages, I could physically feel the depletion of energy. Like your energy bank is lowering and various functions are going into shut down mode due to insufficient power. So as they shut down one after another the structure weakens as a whole.”
“Steadysnacks”
“Sometimes after just talking on the phone, I am almost in tears as my muscles cave and weaken, my eyes become heavy, my heart is erratic, my body becomes extremely uncomfortable, and my brain no longer functions properly. I go from feeling functional to bedridden until my battery is recharged. I can lose days that I thought were going to go well.”
Do any of these descriptions resonate with you? Those are just a few examples recently shared with us. We hope that helps describe the reality of PEM. Thanks to the people with ME and Long Covid who shared. We would love to hear your descriptions.
Final Thoughts
We must mention #StopRestPace if discussing PEM. PEM is why we must stop, rest, and pace. Pacing is a self-management strategy for activity. It is not a treatment or cure but it can prevent further deterioration. When you pace for ME/CFS you are active when able, and resting when tired. Although this level of activity will look radically different from pre-illness levels of activity. You will need to plan extra rest ahead of activities and practice radical rest. It sounds kind of simple when you explain it but it is difficult when put into practice. When you first become ill with PEM through ME, what you can physically do has just radically changed and that means radical adjustments. That is where pacing comes in. The goal is to do as much as you can SAFELY. “Safely” just looks A LOT different.
Wow! You made it to the end. Thanks for reading. We would love to hear what facets of ME you would like featured on future Fridays where we discuss more facets of ME.
- ARTIST CREDIT: Donni Lockridge generously donated this art for #MEAction’s use.
- Check out more on #StopRestPace
- A very handy pacing guide
- Detailed info on PEM
- Learn more about Workwell CPET testing




14 thoughts on “Facets of ME”
This timely Crash Care Survival Guide just came out from Bateman Horne. https://batemanhornecenter.org/wp-content/uploads/filebase/crash_care/B_W_Survival_Guide_Complete.pdf
The Bateman Horne Center Guide is Fantastic! Thank you so much!
Thank you immensely.
My experience with PEM is that it can does does change nature over the course of my illness. What might be delay in cognitive processing these days after allowing myself to become overly stimulated or rundown, was total inability to function or even write a phone number in another decade. The variations within myself are extreme, I can not imagine characterizing them as a criteria.
If we are going to jump to a conclusion that we are in the same boat as Long Covid, why then don’t we include the Fibromyalgia/CFS Population?
I know that I live in a area where my Doctor’s don’t give a ME/CFS diagnosis and many have never heard about it!
We are all given the FM/CFS Diagnosis.
I’ve been on many support groups and the FM/CFS Population have the same symptoms as ME/CFS. We would be many MILLIONS STRONGER as we suffer the same!
Every experience explained was like listening to bird song for the first time. It was so thoughtfully put and it felt like, “thank you. Somebody gets it”.
Thankyou, this is so helpful……. Pacing is hard when there is so much to be done, I mean just
getting breakfast, and preparing supplements and healing potions and drinks……. anxiety
often stops pacing, as taking a rest is hard when anxious….. I often have to forfeit my mental
exhaustion to get some physical rest by doing a Sudoku (when there is so much I should be
sorting through – cleaning up my mess which has built up over the years)…. Sudoku does my
brain in, but makes me lay down…..also, my GP whom I have been going to for years, can’t help
me much with CFS/ME and I understand, but he bulk bills, and helps with forms for Enhanced
Care Plans to go to Physio, Clinical Psychologist. Recently when applying for a Carer’s Allowance
for my friend, he hadn’t supplied enough detail, and I told him not to put just CFS, but CFS/ME,
and he didn’t know what it was or how to spell it, and said they (the govt.) won’t know what it
is.
thanks for this! and the artwork is wonderful!!
I’d like to mention another facet.
What is it they say about the body’s energy use? Something like 70% of it is used running the brain? It’s a lot anyway. So naturally a disease that shuts down our energy when we try to use too much will be affected by mental activity even more than by physical activity, right?
But after almost a decade with ME I can somewhat successfully estimate the price of various physical activities but I’m only just starting to grasp what my limits are for mental exertion. Simple things like reading, I find I can’t continue long enough to hurt myself (though I used to read for hours a day back in my real life, sigh). It’s emotional stress that really beats me up though. Being startled by a sudden noise, worrying about a friend or pet with a health issue, quarrelling with a spouse, anxiety about a big investment like choosing a practitioner to consult, or even good stress like getting a call from a loved one you lost touch with, can cause PEM. In my case at least, the mental PEM is often even worse and longer lasting than the PEM from my physical overexertions!
I keep a log of my activities to help judge if I need to cut back, and this confused me for ages, how I’d get PEM “out of nowhere” when my log didn’t show any unusual exertion. Those were times I’d had a phone call or something else mental, not out of the blue after all! Figuring this out isn’t a total fix because often such things are unavoidable, but at least when you understand how it works you can make yourself rest hard after a mental/emotional stressor, and minimize the PEM.
Thank you Katherine for addressing the emotional stress and overexertion so to speak. For me, stress and distress cause the worst PEM. I have progressive ME – I worsen over time but mostly I have very severe PEM that is permanent and I change overnight. The biggest declines have followed periods of increased stress and emotional upset. And sadly, the sicker I get, now housebound seven years and virtually bedbound after 38 years of illness, the harder it is to cope with things and the easier it is to feel stressed. It’s a vicious cycle!
The worst PEM for me feels like I’m falling down down down into a bottomless pit, I long to reach the bottom so I can rest and recover but the bottom doesn’t come. I’m just falling falling endlessly. It’s such a horrible helpless feeling. “Tired” is so inadequate!
Another analogy….
I feel like I haven’t got the energy to even remain three dimensional. I want to deflate down to nothing like an airbed, just lie on the floor in a pool, flat and empty. Reach oblivion. But I can’t.
I was hoping for something I could share with healthcare practitioners. This doesn’t make the grade. Doesthist have to be this vague and touchy feely, or could it be more “research based”? That would be immensely helpful.
I’d like to add the emotional or mood change that comes with PEM that I experience along with the extreme physical and cognitive declines. It’s like a switch has flipped here too and as I lay on the couch sinking deeper and deeper feeling any remaining life just flow out of me like a popped balloon, my mood has changed dramatically. A few minutes ago I was in good spirits and I was enjoying what I was doing however simple, but when PEM strikes, that goes away too and I feel so bad that I wonder how could I have ever felt in a good mood? I doubt myself – did I really feel that way because I sure don’t now? When I have PEM, it’s not just a worsening of this illness and functioning but a qualitatively different way of being, much worse obviously.
One more word or warning about PEM and pacing. I got sick in the 1980’s and we didn’t know anything about PEM. And I did what comes naturally – I pushed and pushed myself. I rested a lot often because I had to. I couldn’t go on. For about 18 years, my level of illness and functioning were overall ‘stable’ with frequent ‘flare ups’ as I called them then. Then this disease changed into a progressive one following a long period of extreme and relentless stress. Now when I get PEM, it’s permanent. I do not improve. I do not go back to my prior level of illness and functioning. And it’s awful. I just keep losing life and myself. Please do not push yourself until you’re tired and then rest. Stop before you’re tired and worn out. Easier said than done. Still difficult after four decades but the consequences are so severe.
All of the above statements are an excellent description. Another thing that often happens with me is an all over feeling of being poisoned. I literally feel like there is some horrible acidic toxin coursing through my veins. At my worst times with this illness I can not stand any noise (earplugs), light bothers me, my body feels weighted down and poisoned. At my sickest times it has felt like i’m dyeing and yet you don’t die, you get to experience these bizzare symptoms over and over for years. PEM is odd too because sometimes it is the strangest thing like mental tasks or emotional issues that can set things off. My worst times with this illness have lefy me unable to move or talk, it is truly a feeling of being trapped in your body. Its great to see these videos. I wish it was easy to share the video though. thanks for doing this ME/zction
Comments are closed.