On December 3-4, 2020, the National Institutes of Health (NIH) / National Institute of Allergy and Infectious Diseases (NIAID) hosted a virtual Workshop on Post-Acute Sequelae of COVID-19. We know acute COVID-19 has an extraordinary number of multisystem manifestations: pulmonary, cardiovascular, neurologic, psychiatric, musculoskeletal, endocrine, renal, hepatic, gastrointestinal, and dermatologic. The workshop’s goal was to summarize existing knowledge on post-acute manifestations of COVID-19 (what occurs after two weeks post-infection), identify knowledge gaps, and discuss potential approaches for filling those gaps.
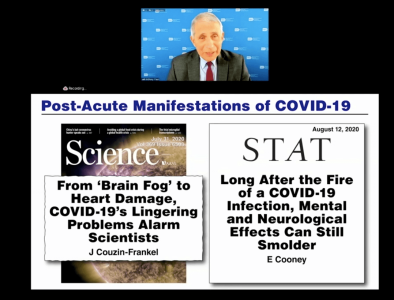
Day 1 of the workshop opened with welcoming remarks by Dr. Anthony Fauci, director of NIAID. He emphasized that post-acute COVID sequelae – also known as long COVID – is a real phenomenon characterized by long-term multisystem symptoms. Dr. Fauci stated, “Given the massive number of SARS-CoV-2 infections, even a small proportion of people who go on to develop post-acute COVID sequelae (or post-COVID chronic illness) represents a significant public health issue.” This pandemic’s enormous global burden affords us a unique opportunity to study and understand the post-acute effects following SARS-CoV-2 infection. Dr. Fauci acknowledged that ME/CFS is one of various post-acute COVID syndromes that will need to be considered and further characterized.
The workshop continued with talks and discussions focused on clinical observations (both US and international), including speakers from the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and physician-researchers from the fields of critical care medicine, HIV, and Ebola. Because SARS-CoV-2 is a new virus, clinicians, researchers, and patients will need to engage in a collaborative effort to characterize many aspects of COVID-19: epidemiological, clinical spectrum, natural history, risk factors, and pathogenesis. “We have a very poor understanding of post-acute and long COVID right now,” said Dr. John Brooks, a medical epidemiologist at the CDC’s Division of HIV/AIDS Prevention, “We are hard-pressed to say we know much.”
First of all, it is important to distinguish between the well-characterized post-intensive care syndrome (PICS) (a collection of physical, cognitive, and emotional symptoms that continue to persist after a patient leaves the intensive care unit [ICU]) and the less characterized post-acute COVID syndromes that develop in non-ICU hospitalized and non-hospitalized people. In addition, some people will have sustained organ damage. While symptoms may overlap across various post-acute COVID syndromes, we must delineate and define these syndromes, as well as their underlying pathophysiology. Although initiated by a common event (SARS-CoV-2 infection), pathophysiologic consequences and disease/symptom outcomes differ substantially across individuals and also vary within an individual over time. Moreover, the severity of acute COVID illness does not necessarily predict the presence or severity of post-acute sequelae, as many younger, non-hospitalized people are suffering from persistent symptoms. As the duration of long COVID symptom presentation is also heterogeneous, it is also essential to define what it means to be “recovered” from COVID.
Insights from the patient’s perspective provided expertise on the “lived experience” of long COVID. Dr. Peter Piot, a previously healthy 71-year-old clinician and microbiologist at the London School of Hygiene and Tropical Medicine, said it was even difficult to convince his colleagues he was still sick from COVID months out from his acute infection. His long hauler experience consisted of two hospitalizations within the first month (treating different sets of symptoms) and a prolonged recovery, in which lingering shortness of breath, low oxygen saturation levels, extreme fatigue, and exercise intolerance gradually improved over a 3-4 -month period. Eight months later, he has been able to resume his pre-COVID activity levels but still requires more sleep than before COVID. Sadly, two of the invited “living with COVID” panelists could not attend the workshop due to recent hospitalization.
The remaining “living with COVID” panelists were Chimere Smith and Hannah Davis – two women in their 30s who were not hospitalized (although Chimere, a Black woman, had multiple ER visits). Ms. Smith, a teacher in Baltimore, MD, and Ms. Davis, an artist/composer in Brooklyn, NY and independent researcher with the Body Politic COVID-19 Support Group/ Patient-Led Research for COVID-19, are current activists in their community. They spoke with conviction about the debilitating symptoms they endured for months and the stigma associated with a lack of awareness and not being believed. The latter is especially pertinent to communities of color. They highlighted the prevalence of neurologic, cognitive, and emotional complications of long COVID and their significant impact on one’s everyday functionality, quality of life, and ability to work. Eight months out for them, Ms. Davis shows improvement in her cognitive function but still has memory problems; Ms. Smith has been unable to work since getting sick and has deteriorating health and post-exertional malaise (PEM) – a defining feature of ME/CFS.
Due to the multisystem nature of post-acute COVID sequelae, there is a need to apply integrated, multidisciplinary approaches for the diagnosis, prognosis, treatment, and management of all stages of COVID-related illness. Therefore, in addition to any required physical and occupational therapy to recover lung, cardiac, and musculoskeletal function, post-COVID clinics should serve a crucial role in providing cognitive and mental health therapy and social work services. Community engagement and partnerships with patient advocacy groups are also vital for including diverse populations’ expertise to inform the development of research protocols and healthcare guidance.
The workshop then shifted to a discussion on the pathogenic features of coronaviruses and host immunological responses, as well as the multisystem inflammatory syndrome in children (MIS-C). A multisystem inflammatory syndrome in adults (MIS-A) also has been reported. It is unclear whether MIS-C/A represents a delayed manifestation of acute infection (occurs about 2-5 weeks after initial infection) or an entirely post-acute phenomenon. Longitudinal clinical studies and appropriate pre-clinical models will help investigate the biological mechanisms underlying the transition from acute to post-acute to long-term sequelae of COVID-19.
The first day ended with a series of Post-Acute COVID-19 Perspective talks on various focus areas, to include what is currently known about: 1) neurologic/psychiatric/neuromuscular, 2) cardiovascular, 3) pulmonary, 4) renal/GI/metabolic, 5) immunologic/rheumatologic, and 6) pediatric aspects of acute and post-acute sequelae of COVID-19. This session set the stage for the next day’s breakout groups, where discussion panels dove deeper to identify and address key knowledge gaps regarding the sequelae in their respective focus areas, as well as cross-cutting issues that pertain to multiple focus areas.
Dr. Avindra Nath (intramural clinical director of the National Institute of Neurological Disorders and Stroke [NINDS]) gave the neurologic/psychiatric/neuromuscular Perspective talk. While there wasn’t much focus on “ME/CFS” per se in Dr. Nath’s talk, “ME/CFS” did appear on two of his slides: 1) listing ME/CFS as one of COVID’s post-viral syndromes (along with encephalopathy, encephalitis, MIS-C/A, and dysautonomia), and 2) stating that the multisystem symptoms of long COVID overlap considerably with ME/CFS. As fatigue has been the most common symptom reported in long haulers, Dr. Nath acknowledged that “even small levels of exertion can cause extreme fatigue, leaving one unable to carry on with daily activities.”
ME/CFS was finally brought into the spotlight by Dr. Peter Rowe (Johns Hopkins University Medical School) in his pediatric Perspective talk on Day 1 and during the neurologic/psychiatric/neuromuscular breakout session on Day 2, in which Dr. Anthony Komaroff (Harvard Medical School) was the chair and Dr. Nancy Klimas (Nova Southeastern University) and Dr. Dikoma Shungu (Weill Cornell Medical College) were panelists. It was important to have these four ME/CFS specialists included in this NIH-sponsored forum to give a credible voice to the ME/CFS community. The need for consistent and correct ascertainment for ME/CFS features of long COVID was stressed, including increasing assessment of PEM, dysautonomia/orthostatic intolerance, and joint hypermobility; delineating what symptoms may be due to an underlying dysautonomia; and providing a better definition and breakdown of “brain fog” into its distinct cognitive components. Dr. Rowe also squeezed in the crucial point that graduated exercise therapy (GET) and cognitive behavioral therapy (CBT) are not recommended for the treatment of ME/CFS, and can be harmful in a subset of COVID long haulers with similar symptoms (especially in those with PEM).
Day 2 also included a talk on the impact of social determinants of health, race, and ethnicity on post-acute COVID-19 sequelae, as people of color are experiencing a greater burden of disease and death. Unfortunately, most of what was presented in this session focused on disparities in COVID case numbers and deaths, and not on disparities in the development of post-acute sequelae. Data on the latter are most certainly needed. As the COVID-19 pandemic has made racial and ethnic health disparities even more apparent, there was a charge to implement policy changes to increase socioeconomic equality and healthcare access to help provide greater health equity moving forward.
Terri Wilder, #MEAction’s New York state chapter leader, commented she was disappointed that little about ME/CFS came through in the workshop’s overall summary. Wilder felt, “The committee members and chairs were clearly not listening or paying attention to the details of some of these presentations. Also, there is a difference between (the symptom) ‘chronic fatigue’ and (the complex neuroimmune disorder) ‘ME/CFS.’ When people (clinicians/researchers) are speaking, they need to clarify which one they are talking about. If they are talking about ME/CFS, at least say ‘chronic fatigue syndrome’ not ‘chronic fatigue.'”
Reported Next Steps:
- Compile the knowledge gaps identified in the workshop and make them publicly available in an official report
- Work with CDC, WHO, and other stakeholders to come to a consensus on how to define the heterogeneous collection of post-acute COVID sequelae
- Identify ways to facilitate ongoing collaboration and knowledge sharing between workshop participants
Stay tuned for a more detailed summary of the workshop!
Check out the workshop agenda, speakers, and slides, as well as video segments posted on the NIH VideoCast website (Past Events).
See individual video links below:
- Workshop of Post-Acute Sequelae of COVID-19 (Day 1)
- Workshop of Post-Acute Sequelae of COVID-19 (Day 2)
- Breakout Session 1 (Neurological / Psychiatric / Neuromuscular)
- Breakout Session 2 (Cardiovascular)
- Breakout Session 3 (Pulmonary)
- Breakout Session 4 (Renal / GI / Metabolic)
- Breakout Session 5 (Immunologic / Rheumatologic)
- Breakout Session 6 (Pediatric)